Understanding Anal Fistula Surgery: Steps, Risks, and Recovery
Tuesday, 28th May 2024Anal fistulas can cause significant discomfort and complications if left untreated. When conservative treatments are ineffective, surgery may be necessary. This guide provides an overview of what to expect from anal fistula surgery, including the steps involved, potential risks, and tips for recovery.
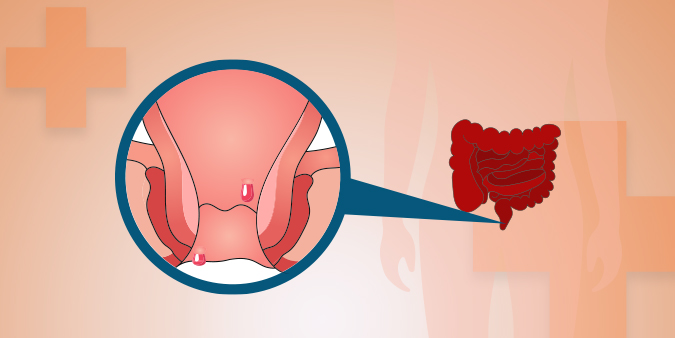
What is an Anal Fistula?
An anal fistula is an abnormal tunnel that forms between the inside of the anus or rectum and the skin around the anus. It usually develops after an anal abscess (a collection of pus) that has not healed properly. Anal fistulas can cause pain, swelling, and discharge, and may lead to recurring infections.
When is Surgery Needed?
Surgery is typically recommended for anal fistulas that:
- Cause significant pain or discomfort.
- Recur frequently.
- Do not heal with conservative treatments, such as antibiotics or drainage.
- Lead to complications like infection or abscess formation.
Types of Anal Fistula Surgery
Fistulotomy
Fistulotomy is the most common surgical procedure for treating anal fistulas. It involves cutting open the entire length of the fistula to allow it to heal from the inside out.
Benefits:
- High success rate.
- Effective for simple fistulas.
Risks:
Seton Placement
A seton is a piece of surgical thread that is placed through the fistula tract to keep it open and allow it to drain. This method is often used for complex fistulas involving the sphincter muscles.
Benefits:
- Reduces the risk of incontinence.
- Effective for complex or high fistulas.
Risks:
- Requires multiple procedures or adjustments.
- Longer healing time.
Advancement Flap Procedure
This technique involves removing the fistula tract and covering the internal opening with a flap of healthy tissue from the rectum.
Benefits:
- Preserves the sphincter muscles.
- Suitable for fistulas involving a significant portion of the sphincter.
Risks:
- Risk of flap failure.
- Requires a high level of surgical expertise.
LIFT Procedure (Ligation of Intersphincteric Fistula Tract)
The LIFT procedure involves accessing the fistula between the sphincter muscles, tying off the internal opening, and removing the infected tissue.
Benefits:
- Low risk of incontinence.
- Effective for complex fistulas.
Risks:
- Risk of recurrence.
- May require additional procedures.
Preparing for Anal Fistula Surgery
Pre-Surgery Consultation
During your pre-surgery consultation, your doctor will:
- Review your medical history and current medications.
- Perform a physical examination and possibly recommend imaging tests, such as an MRI or ultrasound.
- Discuss the type of surgery and what to expect. Provide specific instructions on how to prepare for surgery.
Pre-Surgery Instructions
To prepare for anal fistula surgery, you may need to:
- Stop Certain Medications: Follow your doctor’s advice on which medications to stop before surgery, such as blood thinners.
- Fasting: Avoid eating or drinking for a specified period before surgery.
- Arrange Transportation: Since you may be under anesthesia, arrange for someone to drive you home after the procedure.
- Plan for Recovery: Prepare your home for a comfortable recovery by setting up a rest area and ensuring you have essential supplies on hand.
What to Expect on the Day of Surgery
Before the Surgery
- Check-In: Arrive at the hospital or surgical center as instructed and check in for your procedure.
- Pre-Operative Prep: You will be prepped for surgery, which may include changing into a surgical gown and having an IV line started.
- Anesthesia: You will receive local, regional, or general anesthesia to ensure you are comfortable during the procedure.
During the Surgery
The specifics of the surgery will depend on the type of procedure being performed. Generally, the steps include:
- Incision: The surgeon makes an incision to access the fistula.
- Repair: The fistula tract is either opened, tied off, or removed, depending on the chosen procedure.
- Closure: The surgical site is closed with sutures or left to heal naturally, depending on the type of surgery.
After the Surgery
- Recovery Room: You will be taken to a recovery room to wake up from anesthesia. Your vital signs will be monitored.
- Discharge: Depending on the surgery and your recovery, you may be able to go home the same day or you may need to stay in the hospital overnight.
Recovery After Anal Fistula Surgery
Immediate Post-Surgery Care
- Pain Management: You will be given pain medication to manage any discomfort.
- Activity Restrictions: You will need to avoid strenuous activities and heavy lifting for a specified period.
- Wound Care: Keep the surgical site clean and dry. Follow your doctor’s instructions for wound care and dressing changes.
At Home
- Rest: Get plenty of rest and gradually increase your activity level as advised by your doctor.
- Diet: Follow a high-fiber diet to prevent constipation and ensure smooth bowel movements. Drink plenty of fluids.
- Stool Softeners: Use stool softeners or laxatives as prescribed to avoid straining during bowel movements.
Follow-Up
- Appointments: Attend all scheduled follow-up appointments to monitor your recovery and address any concerns.
- Symptoms: Contact your doctor if you experience severe pain, fever, increased bleeding, or signs of infection at the surgical site.
Long-Term Recovery
- Hygiene: Maintain good anal hygiene to prevent infection and promote healing.
- Exercise: Begin with light exercises, such as walking, and avoid heavy lifting until your doctor gives the go-ahead.
- Lifestyle Changes: Incorporate dietary and lifestyle changes to prevent future fistulas, such as eating a high-fiber diet, staying hydrated, and avoiding straining during bowel movements.
Success Stories: Real Patient Experiences
Sarah’s Relief from Pain
Sarah, a 35-year-old nurse, shares her experience: "After months of dealing with pain and discharge from an anal fistula, I underwent the LIFT procedure. The surgery was straightforward, and the recovery was manageable. I’m now pain-free and back to my normal activities."
Mark’s Journey with Complex Fistula
Mark, a 50-year-old teacher, recounts his journey: "My complex fistula required seton placement. It took a few months and several adjustments, but the procedure worked. The support from my healthcare team was fantastic, and I’m finally free from the recurring infections."
Conclusion
Anal fistula surgery is a common and generally effective procedure for treating chronic anal fistulas. Understanding what to expect and how to prepare can help ensure a smooth and successful outcome. If you are considering anal fistula surgery, consult with your healthcare provider to discuss your treatment options and take the first step towards relief and recovery.


