Anal Fissures Explained: Why They Happen and How to Prevent Them
Tuesday, 28th May 2024Anal fissures are a common condition that can cause significant pain and discomfort. Understanding why they happen and how to prevent them is crucial for maintaining good anal health. This article explores the causes of anal fissures and provides practical tips on how to prevent them.
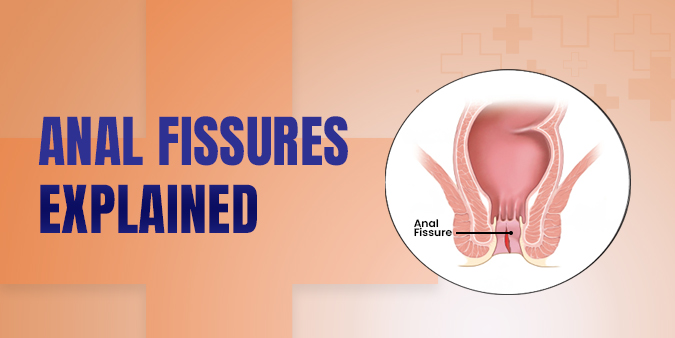
What Are Anal Fissures?
An anal fissure is a small tear or crack in the thin, moist tissue (mucosa) that lines the anus. Fissures can cause severe pain and bleeding during bowel movements. They are often mistaken for other conditions such as hemorrhoids, but they require different treatments.
Why Do Anal Fissures Happen?
Hard Stools and Constipation
Hard stools and constipation are the most common causes of anal fissures. Straining during bowel movements and passing large or hard stools can create small tears in the anal lining.
Chronic Diarrhea
Chronic diarrhea can also lead to anal fissures. Frequent bowel movements can irritate and inflame the anal mucosa, making it more susceptible to tearing.
Childbirth
Childbirth can cause anal fissures, particularly if there is significant straining or tearing during delivery. This is a common cause of fissures in women who have recently given birth.
Anal Intercourse
Anal intercourse can sometimes cause anal fissures due to the potential for friction and tearing of the anal mucosa.
Underlying Health Conditions
Certain underlying health conditions can increase the risk of anal fissures, including:
- Inflammatory bowel disease (IBD): Conditions like Crohn's disease and ulcerative colitis cause chronic inflammation in the intestines, which can extend to the anus.
- Anal cancer: Rarely, anal fissures can be associated with anal cancer.
Other Contributing Factors
Other factors that can contribute to the development of anal fissures include:
- Low-fiber diet: A diet low in fiber can lead to constipation and hard stools.
- Dehydration: Not drinking enough fluids can result in hard stools.
- Poor anal hygiene: Improper cleaning can irritate the anal area, increasing the risk of fissures.
How to Prevent Anal Fissures
Maintain a High-Fiber Diet
Eating a high-fiber diet helps to keep stools soft and regular. Foods rich in fiber include fruits, vegetables, whole grains, and legumes. Aim to consume at least 25-30 grams of fiber per day.
Stay Hydrated
Drinking plenty of water is essential for preventing constipation and maintaining soft stools. Aim to drink at least 8 glasses of water a day.
Practice Good Bowel Habits
Avoid straining during bowel movements. Go to the bathroom as soon as you feel the urge to prevent stool from becoming hard. Do not sit on the toilet for prolonged periods.
Use Stool Softeners
If you are prone to constipation, consider using stool softeners or laxatives as recommended by your healthcare provider. These can help make bowel movements easier.
Maintain Proper Anal Hygiene
Proper anal hygiene can prevent irritation and inflammation. Gently clean the anal area with water after bowel movements and avoid using harsh soaps or perfumed wipes.
Avoid Anal Trauma
Be gentle during activities that could cause anal trauma, such as anal intercourse. Use lubrication to reduce friction and avoid tearing.
Manage Chronic Conditions
If you have an underlying health condition such as IBD, work with your healthcare provider to manage your symptoms and reduce the risk of anal fissures.
Exercise Regularly
Regular exercise promotes healthy bowel function and can help prevent constipation. Aim for at least 30 minutes of moderate exercise most days of the week.
Conclusion
Anal fissures can cause significant discomfort, but understanding the causes and taking preventive measures can help reduce your risk. By maintaining a high-fiber diet, staying hydrated, practicing good bowel habits, and managing underlying health conditions, you can keep your anal area healthy and prevent fissures. If you experience persistent pain or bleeding during bowel movements, consult with a healthcare provider for proper diagnosis and treatment.


